The integration of AI in healthcare is no longer experimental, it’s operational. From streamlining patient workflows to enhancing diagnostic accuracy through medical imaging, AI is changing how healthcare systems work at every level. In an industry where time, accuracy, and coordination can make the difference between life and death, intelligent systems are enabling doctors and hospitals to move faster, decide smarter, and treat better.
Below are 8 transformational use cases showing how AI is reshaping operations and diagnosis—with real-world examples and measurable outcomes.
1. Medical Imaging: From Scan to Signal in Seconds
AI in healthcare has found one of its most impactful applications in medical imaging. Radiologists today face the dual challenge of rapidly rising imaging volumes and increasing complexity in scan interpretation. AI tools are addressing both by turning static images into dynamic diagnostic insights, with consistency, speed, and scalability.
Deep learning models trained on thousands of X-rays, CT scans, and MRIs are now capable of detecting conditions such as pulmonary embolisms, intracranial hemorrhages, and early-stage cancers with remarkable accuracy. Platforms like Aidoc and Zebra Medical Vision have been shown to cut radiologist review times by up to 80%, enabling real-time triage in emergency settings.
AI medical imaging training and inference pipeline (Source: CEUR Workshop on AI in Healthcare)
Behind this performance is a complex model training process. Medical image datasets are processed through convolutional neural networks (CNNs), which extract hierarchical visual patterns – like lesion shape, tissue density, or structural variation. To ensure adaptability in real-world settings, researchers enhance training with synthetic noise, multi-domain inputs, and denoising techniques.
Key methods include:
- Noise-augmented training: Simulates real-world image imperfections to improve model robustness
- Input mixing and fine-tuning: Enhances generalization across different hospitals, devices, and populations
- DCT-based denoising: Cleans low-quality scans to retain diagnostic clarity
- Domain shift adaptation: Ensures the model performs well across varying imaging environments and demographics
Together, these techniques enable AI to operate reliably across telemedicine, rural clinics, and tertiary care centers alike.
AI medical imaging market growth by application, 2020–2030 (Source: Grand View Research)
The market reflects this momentum. In the U.S. alone, AI in medical imaging is projected to grow from $524 million in 2024 to $2.9 billion by 2030, led by neurology, cardiology, and breast screening. This expansion is driven not just by innovation, but by necessity—AI is helping fill diagnostic gaps, support overworked radiologists, and deliver faster, more equitable care.
With AI’s evolving capability to see, interpret, and learn, radiology is shifting from image reading to intelligence orchestration—a leap that redefines what’s possible in diagnostic medicine.
2. Diagnostics Automation: Faster, More Accurate Decisions
In today’s healthcare systems, diagnosis often involves a fragmented and manual workflow—labs processed separately from radiology, and patient symptoms or history scattered across siloed systems. AI in healthcare is transforming this by automating diagnostic reasoning itself: synthesizing vast, multi-source inputs into real-time, actionable insights.
Advanced diagnostics automation leverages multimodal AI frameworks, which integrate both structured data (e.g., lab values, vital signs, medication history) and unstructured data (e.g., doctor notes, radiology reports, free-text symptoms). These models are often built using transformer-based architectures (e.g., MedPaLM by Google DeepMind) or ensemble learning systems that combine deep learning and rule-based logic.
The process begins with data normalization and fusion, allowing the system to build a contextual view of the patient. Using natural language processing (NLP), it interprets physician notes and EHR narratives. Simultaneously, imaging models trained on labeled datasets—such as pathology slides or CT scans—generate visual insights. These results are combined through a diagnostic reasoning engine, often producing differential diagnoses ranked by statistical likelihood and clinical relevance.
Alt text: Healthcare automation challenges in 2025 (Source: Trigent)
Yet while the intelligence is advancing, automation doesn’t operate in isolation. Real-world deployments must overcome persistent friction points in data management, interoperability, third-party integrations, compliance, and technology limitations. For example:
- Inconsistent or poorly labeled EHRs can degrade model performance
- Lack of standardization across hospitals hinders diagnostic model portability
- Automated suggestions must align with local clinical guidelines and regulatory frameworks
Despite these challenges, the benefits are already visible. PathAI, used in digital pathology, has demonstrated over 90% accuracy in identifying cancer subtypes. In primary care, differential diagnosis engines have helped reduce misdiagnosis rates in complex multi-symptom cases like autoimmune disorders or rare infections.
Diagnostics automation isn’t about replacing physicians—it’s about equipping them with an always-on, data-integrating intelligence layer that accelerates clinical clarity and reduces blind spots.
Key mechanisms behind diagnostics automation:
- Multimodal learning: Combines lab, image, and text data into unified diagnostic output
- NLP and transformer models: Extract clinical meaning from unstructured records
- Ranking and reasoning engines: Prioritize potential conditions with explainable probabilities
- Continuous learning: Improves over time with labeled feedback and clinician review loops
As these systems mature, they will become embedded in triage tools, specialist decision support, and even remote consultations—reshaping the pace and precision of diagnosis worldwide.
3. Predictive Analytics: Risk Forecasting That Saves Lives
Among the most transformative uses of AI in healthcare is predictive analytics—the capability to anticipate clinical deterioration, resource demand, or treatment failure before it occurs. Instead of reacting to symptoms, AI enables hospitals to act on what’s likely to happen next, reshaping care from reactive to proactive.
These systems are built on models trained with data from multiple sources: EHRs, wearable devices, health surveys, and longitudinal disease registries. Time-series forecasting, neural networks, and ensemble models detect non-obvious trends across variables like heart rate, oxygen saturation, or blood sugar—often predicting risk windows hours or even days in advance.
In Mount Sinai’s pilot program, AI-driven deterioration prediction led to a 23% drop in ICU transfers and 17% fewer cardiac arrests, proving the value of real-time risk forecasting.
The full pipeline spans from historical data aggregation to real-time monitoring, culminating in continuous predictive outputs. These forecasts are visualized directly within clinical dashboards, helping providers prioritize care across a busy hospital or clinic.
Predictive analytics using patient data to forecast vitals over time (Source: Reveal)
For example, forecasting changes in a patient’s weight or heart rate over 10 years helps clinicians track early signs of cardiovascular or metabolic issues allowing timely intervention long before the patient deteriorates.
At a system-wide level, predictive analytics supports operational improvements: predicting readmissions, optimizing staff allocation, or anticipating surges in emergency care demand.
Use cases of predictive analytics in early detection, clinical decisions, and hospital ops (Source: Wipro)
As the graphic above shows, predictive analytics enhances everything from early disease detection to hospital operations and preventive care. It allows healthcare leaders to anticipate—not just respond—to the shifting needs of patients and populations.
Core methods behind predictive analytics include:
- Data fusion: Merges vitals, medical records, and population data into unified input streams
- Sequence learning models: Captures time-based progression using RNNs or LSTMs
- Risk scoring & stratification: Quantifies risk by probability ranges for each patient group
- Explainable outputs: Supports trust and interpretability in high-stakes decisions
By embedding these tools into daily workflows from nursing dashboards to discharge planning, AI makes early intervention feasible, efficient, and increasingly essential.
4. Virtual Health Assistants and Chatbots: Scaling Patient Access
Virtual health assistants (VHAs) are redefining the patient experience offering real-time, personalized support through conversational AI. Deployed across health systems like the NHS and Cleveland Clinic, these AI-powered chatbots are not just answering questions, they’re streamlining access to care by triaging symptoms, managing appointments, guiding self-care, and even handling post-visit follow-up.
Take Olivia, a virtual health assistant developed for the UK’s NHS. Patients interact with Olivia via voice or text to describe symptoms, receive care guidance, and instantly book appointments—all without a phone call or waiting in line. By layering symptom checking, service location, and scheduling into one seamless interface, Olivia represents a shift from fragmented access to intelligent, user-centered care coordination.
Olivia, NHS virtual assistant app offering symptom checker, bookings, and service locator (Source: NHS/Sensely)
Behind these interfaces lies a modular AI framework. Using natural language understanding (NLU), speech recognition, and dynamic intent parsing, VHAs can extract patient needs, access medical knowledge bases, and route users appropriately. Integration with EHRs, scheduling systems, and external APIs allows these assistants to personalize interactions based on patient history or provider availability.
AI architecture for virtual assistant systems using channels, knowledge bases, and custom skills (Source: Microsoft Industry Blog)
As shown in the architecture above, modern VHAs function as AI-powered orchestration engines, combining:
- Speech-to-text and text-to-speech capabilities for natural interactions
- Conversational AI models trained on healthcare-specific intents and flows
- Customizable skills (e.g., appointment booking, FAQs, symptom triage)
- Access to third-party APIs (e.g., maps, pharmacy locators, calendar systems)
- Multi-channel support via apps, web, SMS, or smart speakers
According to deployment studies, health systems using VHAs saw a 27% reduction in call center volume, improved patient satisfaction scores, and faster routing of urgent cases—all while extending 24/7 support.
These virtual assistants are particularly valuable for underserved populations, non-native language speakers, and patients managing chronic conditions—acting as first-line digital care teams. And as generative AI improves dialog coherence and reasoning, VHAs will evolve from structured Q&A bots into context-aware, emotionally responsive digital companions in everyday care.
5. Remote Patient Monitoring: Real-Time Alerts, Not After-the-Fact Reports
In traditional models, patient data is episodic—captured only during clinic visits. But with the rise of Remote Patient Monitoring (RPM) powered by AI, healthcare is entering a continuous care paradigm. Patients are now monitored 24/7 through connected sensors, while AI translates streams of real-time data into early warning signals for clinicians.
AI-powered RPM systems ingest signals from wearable or implantable devices—tracking vitals like heart rate, blood pressure, oxygen saturation, body temperature, and even gait or sleep patterns. These signals are then analyzed by machine learning models to detect deterioration patterns, anomalies, or deviations from expected baselines.
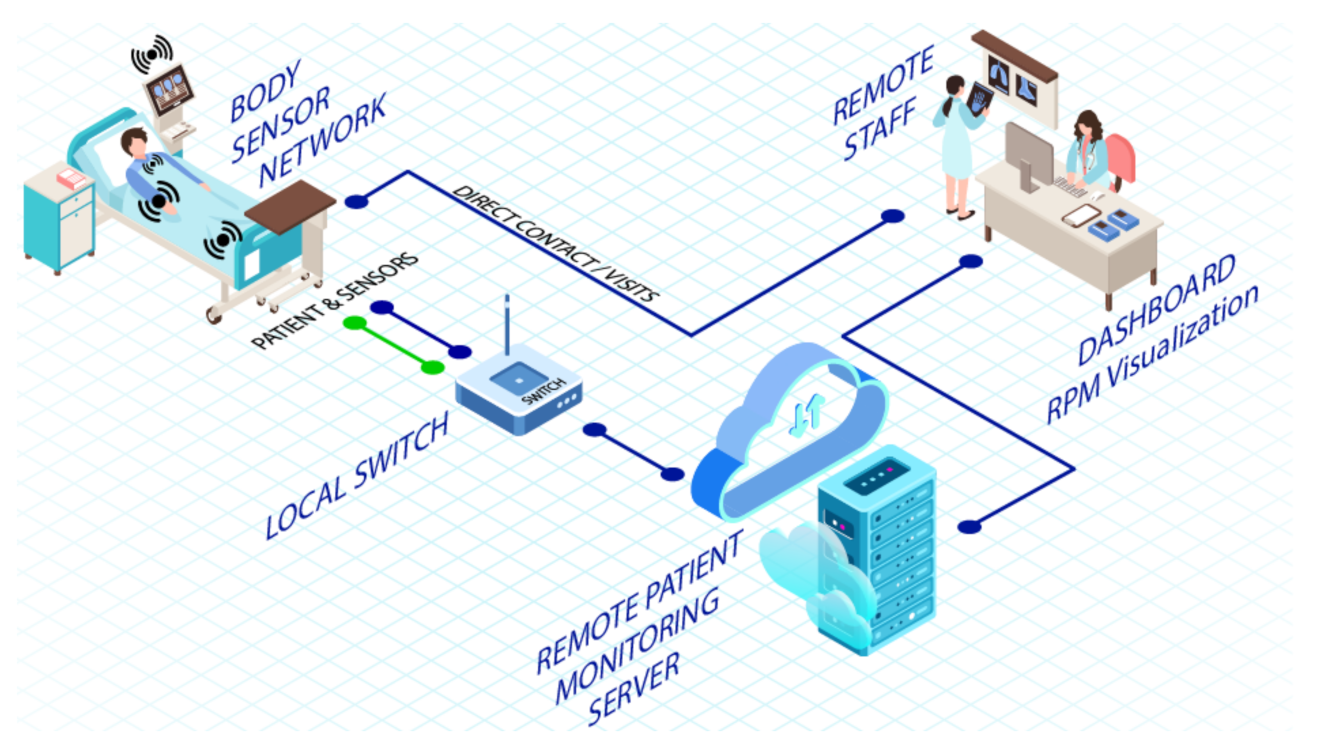
Remote patient monitoring system with sensors, cloud AI, and clinical dashboards (Source: MDPI)
In the infrastructure shown above, body sensors transmit data via local gateways to cloud servers, where AI runs anomaly detection and trend forecasting. Clinicians interact with the system through real-time dashboards, receiving alerts when patient health patterns deviate from personalized baselines. At Mayo Clinic, this model helped reduce heart failure readmissions by 25–30%, as AI flagged early fluid retention long before traditional symptoms appeared.
Remote Patient Monitoring isn’t just convenient—it’s transforming care for chronic illness, elderly patients, and those recovering at home. Rather than waiting for deterioration, healthcare teams can now act with precision, guided by data that never sleeps.
Key AI functions in RPM:
- Detects anomalies in vital signs in real time
- Adapts to patient-specific baselines to reduce false positives
- Forecasts clinical deterioration before symptoms escalate
- Supports clinician decisions with continuous, visualized insights
6. Personalized Treatment Planning: Precision Over Protocol
One of the most profound contributions of AI in healthcare is the shift from standardized treatment protocols to personalized, data-driven care plans. AI enables clinicians to tailor therapies based on a patient’s unique genetic profile, lifestyle data, prior medical history, and response to past interventions—rather than relying solely on generalized clinical pathways.
Advanced AI platforms like Tempus and IBM Watson Health are already in use to support oncologists in selecting the most effective drugs based on tumor genomics. These systems analyze thousands—even millions—of historical treatment records and outcomes, then match patients with the therapy combinations most likely to succeed. In practice, this has helped improve therapy adherence by 30% and reduce adverse drug reactions by 20%, according to Alation’s analysis.
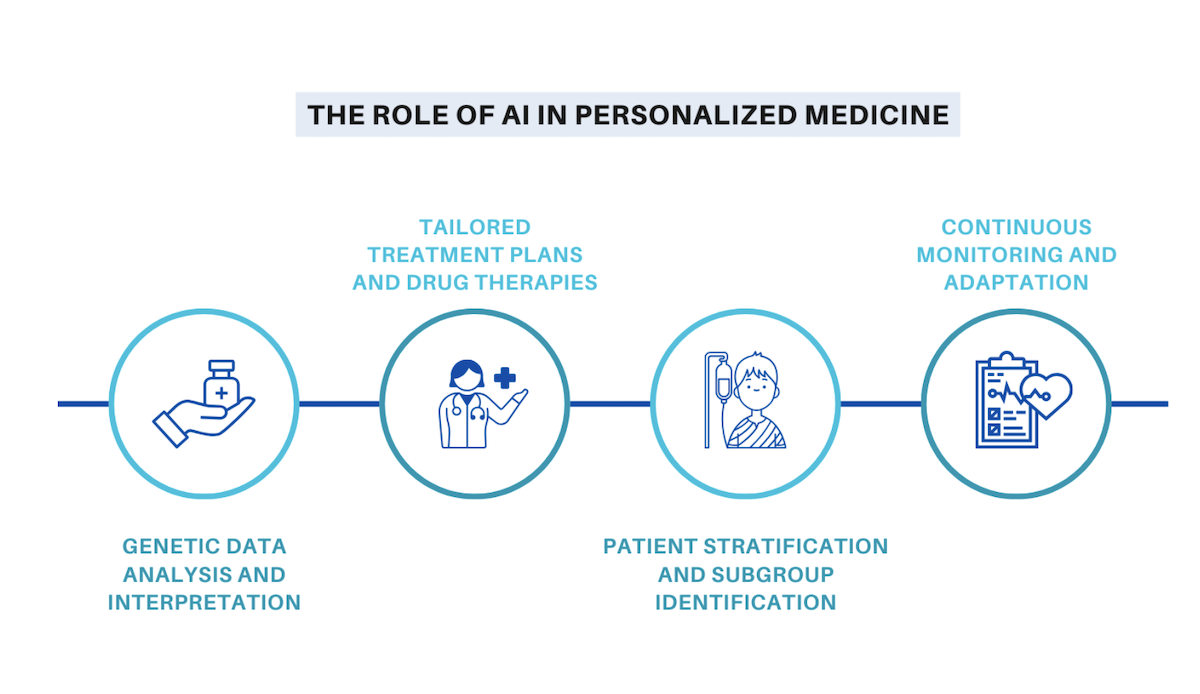
Key steps in AI-driven personalized treatment planning from genomics to monitoring (Source: Insurance Thought Leadership)
As shown above, the process involves multiple AI-driven layers: genetic data interpretation, patient subgroup identification, dynamic care planning, and ongoing adaptation. This continuous loop enables clinicians to refine treatments over time based on real-world patient responses—not just initial diagnosis.
Key AI functions powering personalized treatment:
- Analyzes genomics and proteomics for therapy selection
- Segments patients into molecular or behavioral subgroups
- Recommends optimal drug combinations and dosages
- Adjusts care plans in real time based on biometric and outcome data
Ultimately, personalized medicine with AI isn’t just about customization—it’s about maximizing treatment effectiveness while minimizing risk, cost, and patient burden.
7. Robotic Surgery: Enhancing Human Dexterity with AI
AI-powered robotic surgery combines mechanical precision with advanced decision support, enabling procedures that are less invasive, more accurate, and safer for patients. Platforms like the da Vinci Surgical System interpret a surgeon’s hand gestures while applying motion scaling, tremor suppression, and real-time imaging overlays. This synergy reduces human error and extends surgical capabilities beyond physical limitations.
AI’s role extends beyond assistance. It now supports autonomous planning, guiding incision points and optimizing instrument trajectories. Feedback systems continuously monitor tissue resistance and instrument position, while predictive algorithms suggest adjustments to reduce complications. Some systems have advanced into semi-autonomous tasks such as suturing and cauterization, helping surgeons handle repetitive, high-precision steps with efficiency.
Alt text: Workflow of robotic surgery integrating AI planning, human supervision, and machine feedback (Source: Robotic Surgery Framework Visualization)
As the diagram shows, robotic surgery integrates several layers: intelligent diagnosis, AI-driven surgical planning, real-time human-robot interaction, and post-surgical monitoring. These systems not only assist in the operating room but also create feedback loops to improve performance over time, making each procedure smarter than the last.
According to HealthTech Magazine, robotic-assisted surgery reduces average hospital stays by 1.8 days and lowers complication rates across multiple specialties.
For a deeper discussion on how AI in surgical tools intersects with regulation and risk, explore: Should AI Be Regulated Like Medicine or Like Software?
Key AI functions in robotic surgery:
- Autonomous surgical planning and path optimization
- Real-time force feedback and tissue safety monitoring
- Motion scaling and tremor elimination for ultra-precise movements
- Post-surgical learning loops for continuous performance improvement
8. Administrative Workflow Optimization: Clearing Bottlenecks
Healthcare professionals lose up to 40% of their workday to administrative tasks—charting, coding, billing, and scheduling. AI is now stepping in to automate these burdens through a blend of natural language processing, robotic process automation (RPA), and predictive modeling.
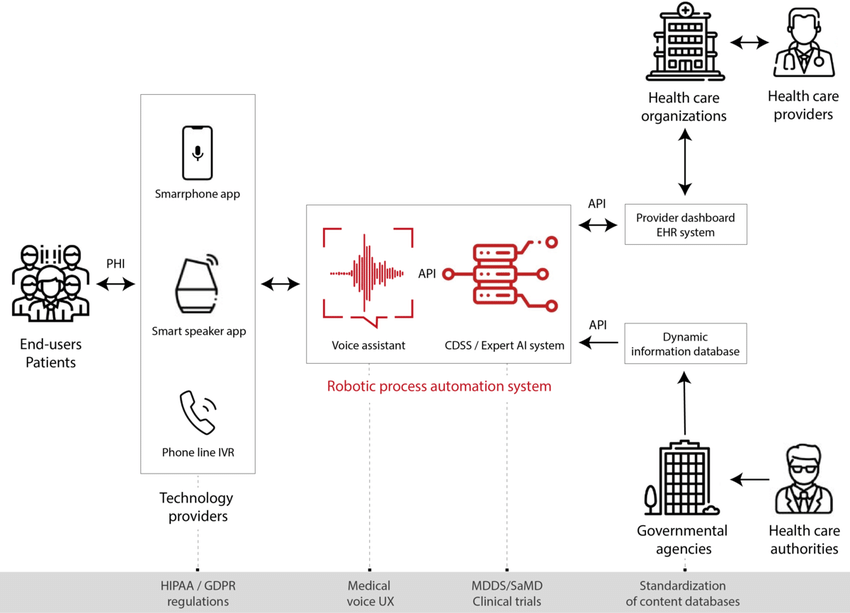
AI automation from patient input to EHR integration and healthcare dashboards (Source: Clinical RPA System Visualization)
As the diagram illustrates, AI-enabled systems now extract data from voice or app-based interactions, route it through expert decision systems, and sync outputs directly with provider dashboards and EHR systems. This streamlines everything from appointment scheduling to insurance pre-authorizations and claim submission. Meanwhile, compliance with HIPAA or GDPR regulations is handled by integrated safeguards in the AI workflow.
Hospitals using AI-driven billing and documentation systems have reported revenue cycle acceleration by 15–20%, along with major improvements in workforce efficiency and clinician satisfaction.
AI in patient workflow isn’t just about speed, it’s about restoring time to care teams, minimizing errors, and ensuring that healthcare delivery scales without burnout.
Conclusion
AI is no longer an experimental layer in healthcare, it’s becoming foundational. From diagnostics to workflow optimization, its value lies in making systems faster, more adaptive, and more personalized. These eight use cases show how AI doesn’t just support care, it reshapes how it’s delivered, coordinated, and scaled.
Still, impact depends on more than algorithms. It requires strong clinical alignment, ethical safeguards, and infrastructure that can evolve alongside the technology. The real opportunity isn’t just automation, it’s building smarter, more resilient systems where intelligence is part of the design.Ready to turn healthcare AI into real, scalable advantage? Visit Twendee Labs, follow us on X, or connect via LinkedIn.